Воспалительная реакция в почечном трансплантате оказывает сильное влияние на начальную и дальнейшую функцию трансплантата. Главными причинами воспалительного процесса в трансплантате служат ишемическое/реперфузионное повреждение (ИРП), эпизоды отторжения трансплантата и инфекция. ИРП ухудшает начальную функцию и отрицательно сказывается на долгосрочных результатах трансплантации почки. Помимо этого тяжелое ИРП может повышать риск развития острого отторжения, что в свою очередь усиливает травму трансплантата.
Стратегия уменьшения ИРП трансплантата может быть поделена на пред- и посттрансплантационную.
Предтрансплантационная стратегия, ослабляющая ИРП, включает сокращение времени холодовой ишемии путем оптимизации транспортировки (логистики) трансплантата, применения «машинной» перфузии или особых консервирующих растворов. Используется кондиционирование доноров с растворами, способными уменьшать ИРП.
Стратегия сохранения органов
Гипотермическая консервация на сегодняшний день остается стандартной процедурой, направленной на уменьшение повреждения трансплантата. Эффективность добавления новых препаратов к существующим консервирующим растворам находится в стадии исследования [1, 2]. Например, ингибитор p38 MARK FR167653, коллоидный полиэтиленгликоль, сокращает истощение АТФ и подавляет аккумуляцию кальция в клетках. Этот препарат успешно использован для уменьшения ИРП после трансплантации [3, 4].
Интересные экспериментальные данные получены при использовании AMФ-активированных протеинкиназ (AMPK). Нарушение клеточного гомеостаза, воспаление и эндотелиальная дисфункция являются последствием повреждающего воздействия патогенных факторов в ходе холодовой ишемии. Истощение АТФ и анаэробный метаболизм в течение периода холодовой ишемии приводят к митохондриальной дисфункции, нарушают осморегуляцию и в конечном итоге ведут к гибели клетки. После конверсии аденозина в AMФ (аденозинмонофосфат) активируется AMPK. Экспериментальная фармакологическая активация AMPK демонстрирует способность к активации эндотелиальной синтазы нитрида азота и подавлению нуклеарного фактора – каппа В (NF-κB), что приводит к уменьшению эндотелиальной дисфункции и воспаления. Активация AMPK перед или в течение консервации органов может быть использована как новый метод фармакологического воздействия, ограничивающий выраженность повреждения трансплантата и снижения его функции [2].
Кондиционирование донора
Некоторые вмешательства способны значительно улучшать состояние органов потенциального донора. Причем кондиционирование донора может быть более эффективным, если оно начинается перед постановкой диагноза смерти мозга. Однако это может быть связано с этическими и юридическими трудностями.
В данном контексте было опубликовано исследование кондиционирования донора с применением дофамина [5].
В этом рандомизированном исследовании авторы кондиционировали доноров после установки смерти мозга с использованием дофамина. В результате функция трансплантата была улучшена, а после трансплантации было сокращено время пребывания реципиента на гемодиализе. Авторы связывают этот эффект с защитой эндотелиальных клеток в течение холодовой консервации от кислородного стресса, т.к. гипотермическая смерть клетки и внутриклеточная аккумуляция кальция при использовании дофамина тормозятся. Подобные положительные эффекты наблюдались среди реципиентов с трансплантированным сердцем, полученным от доноров, пролеченных дофамином [6].
Гипотермическая машинная перфузия
Гипотермическая ex vivo перфузия трансплантата с использованием машин для перфузии исследуется в течение многих лет. Клинические исследования показали, что таким образом можно добиваться лучшей функции почечного трансплантата и уменьшения периода его восстановления [7–9]. Это подтверждается данными мета-анализа: достигаются не только лучшие результаты трансплантации, но и снижаются затраты на содержание реципиента в долгосрочной перспективе по сравнению со стандартной процедурой холодовой консервации трансплантата [10–11].
Нормотермическая консервация
Нормотермическая консервация может обладать высоким потенциалом, поскольку ей не свойственны характерные для холодовой консервации проблемы [1, 12]. Нормотермическая консервация не только сохраняет орган, но и обеспечивает основу для лучшего восстановления функций трансплантата по сравнению с гипотермическими методами консервации. Основные принципы такого подходы заключаются в обеспечении физиологичного «окружения» трансплантата в течение периода хранения, использовании специфических перфузионных растворов. Нормотермическая перфузия может быть выполнена несколькими способами, включая использование крови донора с применением экстракорпоральной оксигенации. Этот метод может быть применен при трансплантации сердца, печени и почек [13].
Посттрансплантационная стратегия
Посттрансплантационная стратегия, снижающая ИРП, включает использование субстанций, вмешивающихся в воспалительный процесс, главным образом через взаимодействие с хемокинами, цитокинами и лейкоцитарной инфильтрацией. С другой стороны, стратегия внедрения в апоптотические процессы была исследована с целью предупреждения гибели клеток и таким образом – защиты трансплантата от дополнительной потери клеточной массы. Идеальным вмешательством может быть короткий курс лечения в течение непосредственно перитрансплантационного периода, приводящий к длительному эффекту.
Серьезной практической проблемой в профилактике/лечении ИРП остается обстоятельство, согласно которому многие терапевтические решения были успешно разработаны на экспериментальных моделях и только некоторые из них применяются в клинических исследованиях [4].
Терапевтические стратегии, применяемые при лечении ИРП
Стратегия профилактики и лечения ИРП включает блокаду цитокинов и хемокинов, молекул адгезии, NF-κB, специфических MAP-киназ, металлопротеиназ, а также индукцию протективных генов.
Цитокины и хемокины
Большинство провоспалительных хемокинов (см. таблицу), таких как IL-8, MCP-1, ENA-78 (epithelial-derived neutrophil-activating peptide 78), MIP-(macrophage inflammatory protein)-1α, MIP-1β или RANTES, требуют активации посредством транскрипционных факторов, таких как NF-κB, или активатора протеина-1 (AP-1) [14–17]. Центральной киназой, необходимой для активации этих транскрипционных факторов, является p38 MAPK (p38 mitogen-activated protein kinase). Ингибиторы этой киназы сокращают провоспалительную цитокиновую продукцию и уменьшают ИРП на экспериментальных моделях с гипоксией [18–20].
Генерация хемокинов увеличивается уже через несколько часов после реперфузии. Ингибирование каспаз, особенно каспазы-1, NF-κB, p38 MAPK, участвующих в генерации хемокинов, эффективно ослабляет ИРП в экспериментальных моделях посредством уменьшения генерации хемокинов [14–17]. Однако для уменьшения действия хемокинов недостаточно только блокирования их продукции.
Одним из перспективных направлений служит использование молекулы Met-RANTES, производной к хемокину RANTES, которая блокирует его действие на уровне рецептора. Лечение Met-RANTES в ранний период – от 0 до 10 дней после трансплантации, когда ИРП наиболее выражено, приводит к ослаблению развития фиброза в трансплантате при использовании экспериментальных моделей на крысах [21–24]. Этот эффект достигается благодаря тому, что уменьшается активность воспалительной реакции после трансплантации. Подобный эффект также имел место при применении блокаторов MCP-1 и MIP в экспериментальных моделях ИРП [15, 16].
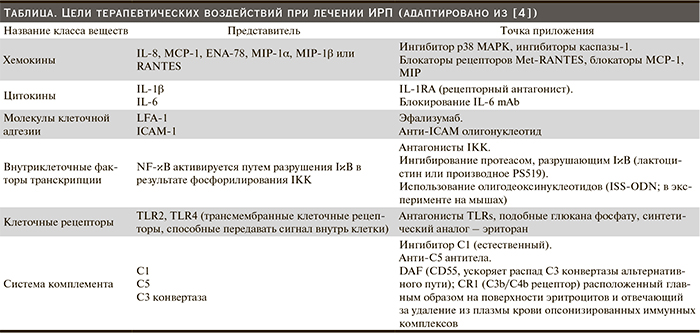
Помимо хемокинов ключевую роль в ИРП после трансплантации играют цитокины (см. таблицу). Особо следует отметить провоспалительный цитокин интерлейкин-1β, медиатор воспаления и иммунитета. Он индуцирует хемотаксис полиморфноядерных лейкоцитов и макрофагов, пролиферацию эндотелиальных и В-клеток [25, 26]. IL-1β индуцирует экспрессию адгезивных молекул на эндотелиальных клетках, обеспечивая таким образом клеточную инфильтрацию. Более того, этот цитокин через увеличение экспрессии циклооксигеназы индуцирует продукцию простагландинов и таким образом повышает число циркулирующих нейтрофилов и тромбоцитов. Действие IL-1 физиологически подавляется IL-1RA (рецепторный антагонист). Были проведены исследования на крысах с применением IL-1RA и доказана его эффективность в плане значительного уменьшения ИРП почечного трансплантата [27–29].
Один из ярких представителей группы провоспалительных цитокинов – IL-6. Он стимулирует пролиферацию кроветворных клеток-предшественников, дифференцировку и созревание Т- и В-лимфоцитов (фактор стимуляции В-клеток 2), вызывает агрегацию тромбоцитов, пролиферацию сосудистых гладкомышечных клеток, опосредует синтез и выделение С-реактивного белка, фибриногена и других белков острой фазы воспаления гепатоцитами, способствует экспрессии тканевого фактора, белка хемотаксиса моноцитов-1, молекул адгезии и других хемокинов (ICAM-1, VCAM-1, CXCL1, CXCL5, CXCL6, CXCL8, CCL2 и др.), препятствует апоптозу нейтрофилов [30]. При дефиците IL-6 повышается устойчивость трансплантата к ИРП [31]. Блокирование IL-6 моноклональными антителами (mAb) или создание искусственного дефицита IL-6 у крыс приводит к снижению тяжести ИРП почек. Выражается это в уменьшении степени нейтрофильной инфильтрации ткани почки, снижении продукции IL-1β, фактора некроза опухоли-α (TNF-α), экспрессии ICAM-1, P-селектина [32, 33].
Другим способом ослабления ИРП служит использование субстанций, которые модулируют противовоспалительные реакции и могут обеспечивать ренальную защиту. Например, экспериментальное введение ИЛ-10, мощного противовоспалительного цитокина, обеспечивало нефропротекцию путем ингибирования синтеза цитокинов Th1-клетками [34–36].
Молекулы адгезии
Молекулы адгезии (см. таблицу) играют важную роль в активации функций воспалительных клеток. ICAM-1 (межклеточная адгезивная молекула 1) участвует в адгезии с LFA-1 (leukocyte function associated antigen 1), что приводит к миграции лейкоцитов к очагу воспаления. Экспериментальные данные говорят о следующем: снижение экспрессии адгезивных молекул тормозит развитие ИРП после трансплантации почки [37–39].
LFA-1 выполняет различные функции в иммунном ответе, среди них адгезия и перемещение лейкоцитов, стабилизация MHC-Т – клеточного рецепторного комплекса, обеспечение костимулирующих сигналов. В клинической практике при трансплантации почки с хорошим эффектом используют эфализумаб – гуманизированные моноклональные антитела (иммуноглобулины класса IgG1), специфически связывающиеся с CD11 α-субъединицей LFA-1 (антигена-1, связанного с лимфоцитарной функцией) [40, 41].
Другая важная молекула адгезии – ICAM-1. Проводились клинические исследования на мышах с применением анти-ICAM-1 олигонуклеотида. Отмечено незначительное уменьшение частоты острых кризов отторжения по сравнению с традиционными иммуносупрессивными протоколами [37, 38, 42].
Интегрины-1β, участвующие в межклеточной адгезии, перераспределяются при ИРП по направлению к апикальной части клетки эпителия канальца и взаимодействуют через интегриновый рецептор Arg-Gly-Asp (RGD). Введение синтетического RGD сопровождается уменьшением интратубулярной обструкции при ИРП. Дальнейшие исследования показали, что доишемическое внутривенное введение моноклональных антител против активированных интегринов-1β (HUTS21) сопровождается сохранением гистологической структуры и функционального состояния межклеточных связей и уменьшением воспалительной реакции [41, 42].
Интервенция в ингибирование NF-κB
Ингибитор κB (IκB) киназного комплекса IKK активируется посредством NF-κB – индуцирующей киназы (NIK), которая активируется TRAF-2 (TNF-рецептор-ассоциированный фактор 2) и RIP (рецептор-взаимодействующий протеин, обладает энзиматической активностью). IKK фосфорилирует IκB, приводя к его разрушению и позволяя NF-κB транслоцироваться к ядру для активации транскрипции [43]. Специфические антагонисты ингибитора киназного комплекса уменьшают ИРП в экспериментах [44].
Другой путь, ведущий к ингибированию IκB деградации, – это подавление отвечающих за разрушение протеасом. При ишемии почечного трансплантата повреждение может быть предотвращено использованием ингибитора протеасом лактоцистина, который следует вводить перед началом ишемии [45].
В экспериментальных протоколах были проанализировали эффекты генной терапии, направленной на подавление NF-κB ядерной транслокации [43]. Однако этот подход не был применен в более крупных клинических исследованиях.
В экспериментальных моделях ИРП показано, что предварительное введение эритропоэтина способствует структурной и функциональной защите клеток канальцев, торможению апоптоза и регуляции антиапоптотического ядерного фактора транскрипции NF-κB [46].
Система врожденного иммунитета, Толл-подобные рецепторы (TLRs)
Было продемонстрировано, что генетическое истощение TLR-2 [47] и TLR-4 [48, 49] в экспериментальных моделях ИРП приводит к значительному ослаблению повреждения тканей по сравнению с контрольной группой. Это было подтверждено недавним клиническим исследованием, в котором трансплантаты с дефектной TLR-сигнальной функцией имели лучшую, чем обычные трансплантаты без повреждения сигнальной функции TLRs, функцию и сниженную экспрессию провоспалительных цитокинов после трансплантации [49]. Характерно, что в экспериментальных моделях ИРП одновременная блокада TLR-2 и TLR-4 не приводила к значительному усилению протективного эффекта [48].
Система комплемента
Система комплемента (см. таблицу) состоит из различных компонентов, которые активируются под действием разнообразных стимулов: инфекционных бактериальных агентов, вирусов, неинфекционных воздействий, среди которых основным является ИРП [50, 51].
Активация системы комплемента приводит в первую очередь к связыванию ее компонентов c определенной структурой, такой как бактерия или поврежденная клетка; хемотаксические свойства некоторых компонентов могут привлекать воспалительные клетки в зону повреждения и разрушать клетки-цели посредством особых литических механизмов.
Ингибирование системы комплемента является эффективным методом ослабления ИРП в экспериментальных моделях [52–54]. В частности, его уменьшает блокирование С5-компонента системы комплемент [55, 56]. Однако снижение тяжести ИРП путем блокады системы комплемента должно быть подтверждено в крупных клинических исследованиях.
Протективные гены
Клеточные процессы могут регулироваться т.н. протективными генами. Их экспрессия увеличивается, когда клетка находится в поврежденном состоянии, и защищает ее (клетку) от запрограммированной гибели (апоптоза) и воспалительного повреждения (путем ингибирования NF-κB). Сверхэкспрессия Bcl-2 (внутриклеточный белковый фактор) подавляет апоптоз во многих клеточных системах, контролируя проницаемость митохондриальной мембраны, ингибирует каспазы за счет предотвращения выхода цитохрома С из митохондрий и/или за счет связывания фактора, активирующего апоптоз (APAF1) [4, 57], и гемоксигеназы-1 [58, 59]. Это значительно ослабляет повреждение тканей в различных экспериментальных моделях ИРП, в т.ч. после трансплантации.
Подавление апоптоза представляется важным аспектом протекции тканей, т.к. ингибирование каспаз также в значительной степени уменьшает ИРП в результате заметного снижения воспалительного ответа [60, 61]. Отмечено, что подавление апоптоза не только предотвращает гибель клетки, но и ассоциируется с уменьшением выраженности воспаления. С другой стороны, апоптозу способствуют mTOR-ингибиторы, в эксперименте они применялись в раннюю фазу после трансплантации почки и усугубляли ИРП [62, 63].
Интересное исследование проведено А. Kezic и соавт., изучавшими иммуномодулирующие свойства рапамицина (mTOR-ингибитора) и влияние эверолимуса на NF-κB-активацию при ИРП [64]. В этой работе эверолимус назначался мышам за 24 часа до трансплантации. Оценивались активность NF-κB, концентрации провоспалительных цитокинов IL-1β, TNF-α и противоспалительного цитокина IL-10. По сравнению c контрольной группой животных у мышей, получавших эверолимус, отмечено значительное повышение уровней TNF-α и IL-1β на 2-е сутки после ишемии/реперфузии. Через 2 часа после ИРП у мышей, получавших эверолимус, наблюдали значительное повышение экспрессии мРНК IL-1β, после чего следовало возрастание концентрации IL-1β. Эти данные свидетельствуют о следующем: эверолимус сильно влияет на врожденный иммунитет в раннюю фазу ИРП и стимулирует продукцию провоспалительных цитокинов – TNF-α и IL-1β. Активность NF-κB в ходе ИРП под воздействием mTOR-ингибирования потенцировалась [64].
Большого внимания заслуживает цинк-связывающий протеин А20 (ЦСП-А20) – молекула с потенциальным протективным эффектом, обладающая антиапоптотическим и противовоспалительным действиями [65]. ЦСП-А20 регулирует рецептор-опосредованный апоптоз (например, через TNF-α) посредством модуляции каспазы-8 и оказывает противоспалительные эффекты за счет подавления NF-κB и TLR-4 [66]. Была проанализирована гиперэкспрессия ЦСП-А20 в моделях ИРП печени и почек [67, 68]. Как оказалось, такая гиперэкспрессия приводит к значительному ослаблению ИРП в обеих моделях, что было обусловлено снижением активации NF-κB, а также уменьшением экспрессии молекул адгезии.
В модели печеночного трансплантата гиперпэкспрессия ЦСП-20 приводила к лучшей его регенерации и сокращению числа эпизодов отторжения, а также к повышению выживаемости трансплантата [69]. Однако до сих пор нет клинического опыта применения этого препарата после трансплантации почки.
Экстрацеллюлярный матрикс в процессе ИРП
Экстраклетоный матрикс играет важную роль в функции почечного трансплантата. Он повреждается посредством матриксных металлопротеиназ (MMPs). В экспериментальных моделях ИРП ингибирование MMPs значительно ослабляет повреждение тканей [70, 71].
Вмешательство в воспалительный процесс на ранней стадии может оказывать протективный эффект, несмотря на то что специфическое лечение уже было прекращено. Причиной этого эффекта может быть ослабление деградации базальных мембран, так же как и других экстрацеллюлярных матриксных компонентов. В результате сохраняется структура тканей и уменьшается инфильтрация тканей воспалительными клетками [72].
Ингибиторы индуцированной синтазы оксида азота
Роль оксида азота и его синтазы интенсивно исследуется. В частности, in vivo и in vitro изучается возможный эффект ингибирования синтазы оксида азота как фактора, ослабляющего ИРП [73, 74].
Антиоксиданты и антиоксидантные ферменты
Избыточная генерация активных форм кислорода (АФК), уменьшение антиоксидантной защиты, как известно, вносят свой вклад в ИРП. Антиоксиданты, направленно блокирующие действие АФК, эффективно используются при ИРП. Эдаравон, связывающий свободные радикалы, увеличивает выживаемость и улучшает почечную функцию крыс, подверженных ИРП. Стобадин, новый синтетический пиридоиндоловый антиоксидант, уменьшающий перекисное окисление липидов и повреждение белка благодаря захвату АФК и повышению антиоксидантной активности, способен в значительной степени снижать тяжесть ИРП почек у крыс [75, 76].
Тромбомодулин и активированный протеин С
Протеолитическая активация протеина С происходит в эндотелиальных клетках благодаря двум мембранным рецепторам – тромбомодулина и эндотелиального протеина С (EPCR). Связывание тромбина с тромбомодулином повышает антикоагулянтные свойства антигенпредставляющих клеток благодаря образованию тромбин-тромбомодулинового комплекса и усилению связывания протеина С с EPCR.
В дополнение растворимый тромбомодулин независимо генерируется антигенпредставляющими клетками и ослабляет ИРП [77]. В этом исследовании растворимый тромбомодулин не только уменьшал подъем концентрации креатинина после реперфузии, но и снижал микрососудистую эндотелиальную лейкоцитарную адгезию, минимизировал эндотелиальную проницаемость.
Мезенхимальные стволовые клетки
Эти клеточные элементы обладают антиоксидантными свойствами, ослабляющими ИРП почечного трансплантата. Мезенхимальные стволовые клетки, полученные из пуповины человека (т.н. микрососудистые дериваты), облегчают оксидативный стресс. Более того, столовые клетки уменьшают фиброз и улучшают функцию почечной ткани [78–81].
Лекарственные средства, ослабляющие цитотоксичность при ИРП
Фармакологическая терапия в качестве средства профилактики и лечения ИРП не слишком эффективна, несмотря на хорошие результаты доклинических исследований. Успех профилактики и лечения этого сложного процесса зависит от понимания его патогенеза, и, таким образом, соответствующая рациональная терапия ИРП может быть реализована в хорошо спланированных клинических испытаниях.
Статины
Использование статинов сопровождается не только уменьшением уровня холестерина, но и противовоспалительным эффектом, снижением генерации АФК, стимулированием образования NO эндотелием, что может быть полезным при защите почек от ИРП.
Дополнительные исследования показали, что противовоспалительная и антиоксидантная активность статинов улучшает эндотелиальную функцию, уменьшает агрегацию тромбоцитов и прокоагулянтных факторов [82]. Правастатин уменьшает подъем уровня креатинина в плазме [83, 84].
Эритропоэтин
В настоящее время эритропоэтин признан фактором, играющим важную физиологическую роль в костном мозге и других тканях. В почках рецепторы эритропоэтина обнаруживаются на клубочковых и интерстициальных клетках. Эритропоэтин ослабляет эндотелиальную дисфункцию и гистологические изменения при ИРП [85–87].
Меланостимулирующий гормон также способен оказывать защитное действие при ИРП путем ингибирования генов, вызывающих воспалительные и цитотоксические повреждения почек, кроме того, усиливает протективный эффект эритропоэтина даже при приеме внутрь после ишемии почек [88–90].
Влияние анестезиологического пособия на ИРП
Восстановление потока крови в трансплантате реципиента приводит к реперфузионному повреждению, которое характеризуется оксидативным стрессом и воспалением.
В настоящее время довольно активно исследуется использование внутривенных общих анестетиков для лечения ИРП органов [91, 92].
Пропофол и изофлюран оказывают положительное влияние при ИРП путем уменьшения воспаления и увеличения антиоксидантной способности трансплантатов [93–97]. Введение изофлюрана мышам за 30 минут до ишемии приводило к снижению уровней сывороточного креатинина и мочевины крови, цистатина С, TNF-α и IL-6 [97].
Функциональные данные коррелируют с гистологическими подтверждениями повреждения почечных канальцев. Тяжелые канальцевые повреждения были найдены у мышей, не подвергшихся влиянию пропофола на фоне ИРП (широкое распространение канальцевого некроза, нарушение целостности эпителиальных клеток, канальцевая дилатация в кортико-медулярной зоне). В то время у мышей, получавших пропофол, повреждения канальцев были менее выражены. Результаты этого исследования могут открыть новые аспекты изучения антиоксидантных эффектов пропофола. Понимание механизмов воздействия пропофола на ИРП можно способствовать внедрению нового метода терапии ИРП [98].
Выводы
ИРП принадлежит главная роль в развитии воспалительной реакции в трансплантате в интра- и раннем посттрансплантационном периодах. Это повреждение оказывает глубокое влияние на первичную и долгосрочную функцию трансплантата. В настоящее время изучено действие множества препаратов, способных снижать тяжесть ИРП. К сожалению, большинство из них не применяется в широкой клинической практике. Данные исследования крайне интересны, поскольку ишемическому, а позже и реперфузионному повреждению в той или иной степени подвержены абсолютно все трансплантируемые органы. Дальнейшее изучение данной проблемы может повышать выживаемость трансплантатов.