Введение
К нейрогенным дисфункциям мочевого пузыря (НДМП) относят разнообразные по форме нарушения резервуарной и эвакуаторной функций мочевого пузыря, развивающиеся вследствие поражения механизмов регуляции мочеиспускания различного генеза и на различном уровне (корковые, спинальные центры, периферическая иннервация) [1].
Дисплазия соединительной ткани (ДСТ) – группа наследуемых или врожденных нарушений соединительной ткани мультифакторной природы, характеризующихся генетической неоднородностью и относительно доброкачественным течением, объединенных в синдромы и фенотипы на основе общности внешних и/или висцеральных признаков [2, 3].
В последние годы большой интерес представляет взаимосвязь между данными состояниями. Показано, что примерно у каждого третьего пациента с ДСТ наблюдаются симптомы, характерные для поражения мочевыделительной системы: частое мочеиспускание, чувство неполного опорожнения мочевого пузыря, никтурия, энурез, симптомы дисметаболической нефропатии, а при углубленном обследовании выявляются поликистоз, дивертикулез мочевого пузыря, нефроптоз, атония чашечно-лоханочной системы, удвоение почки и/или мочевыводящих путей [4–6].
В.А. Гавриловой (2001) показана высокая распространенность ДСТ у детей с нарушениями мочеиспускания: так 2-я и 3-я степени ДСТ выявлены у 72% детей с хроническим пиелонефритом в сочетании с НДМП и у 90% – с изолированной НДМП [5].
Возможно, одним из общих патогенетических механизмов развития нейрогенных расстройств мочеиспускания и диспластического фенотипа являются нарушения вегетативного гомеостаза. Так, для наследственных форм ДСТ было показано, что вегетативная дисфункция является одним из наиболее распространенных симптомов. В целом, по мнению многих авторов, вегетативную дисфункцию следует рассматривать как малый диагностический критерий синдрома гипермобильности суставов [7]. Так, вегетативная дисфункция отмечается в 97% случаев наследственных диспластических синдромов, а при недифференцированной форме ДСТ – у 78% пациентов [8].
По данным Г.И. Нечаева и соавт. (2008), у значительного числа пациентов с ДСТ формируется синдром вегетативной дисфункции. При этом у большинства пациентов выявляется симпатикотония, реже встречается смешанная форма, в малом проценте случаев – ваготония. Выраженность клинических проявлений синдрома нарастает параллельно тяжести ДСТ. С другой стороны, В.Г. Арсентьев (2012) получил отличные данные: по результатам кардиоинтервалографии (КИГ), частота исходной симпатикотонии среди больных ДСТ ниже, чем в контроле (30,7 и 70,8% соответственно, p<0,005), частота ваготонии значимо выше (34,6 и 0%, p<0,005) [9].
Таким образом, формируются предпосылки к изучению особенностей вегетативного гомеостаза, качества жизни у детей, имеющих расстройства мочеиспускания на фоне ДСТ.
Цель исследования: изучить особенности вегетативного гомеостаза и оценить показатели качества жизни у детей с нейрогенными расстройствами мочеиспускания в зависимости от проявлений синдрома ДСТ.
Материал и методы
В наше исследование были включены 26 детей от 5 до 12 лет, средний возраст – 8,3±1,7 года с энурезом и НДМП, находившихся на стационарном лечении в нефрологическом отделении КГБУЗ «Детская городская больница № 1, г. Барнаул».
Критерии включения в исследование: диагноз «энурез», или НДМП, установленный согласно отраслевым стандартам, стационарное обследование, отсутствие наследственных форм ДСТ, отсутствие острых инфекционных и других заболеваний, приема лекарственных препаратов на момент обследования, потенциально оказывающих влияние на вегетативный гомеостаз. У всех больных оценивали анамнез жизни, соматический статус, проводили общеклиническое исследование крови и мочи, функциональные пробы почек. Биохимические исследования включали определение в сыворотке крови содержания общего белка и его фракций, мочевины, креатинина, липопротеидов, холестерина, кальция и фосфора, а также содержание в моче кальция, фосфора, мочевой кислоты и креатинина. Также было проведено ультразвуковое исследование почек и мочевого пузыря, дуплексное сканирование брахиоцефальных сосудов, эхокардиография (ЭхоКГ). По показаниям проводились рентгенконтрастные методы исследования: экскреторная урография и микционная цистография. Степень тяжести расстройств мочеиспускания оценивали по квалиметрической таблице клинической оценки для детей от 4 до 15 лет. ДСТ диагностировали у детей по балльной оценке, ранжированных по значимости, внешним и висцеральным признакам системного вовлечения соединительной ткани. Результат до 12 баллов расценивался как отсутствие дисплазии, 12–20 – дисплазия 1-й степени тяжести, от 20 до 30 – дисплазия 2-й степени, более 30 баллов – 3-й степени. В дальнейшем было сформировано 2 группы сравнения: 1-я – пациенты с дисплазией 1-й степени – 17 детей, 2-я – пациенты с дисплазией 2-й степени тяжести – 9 детей.
Кроме того, проводили оценку качества жизни детей при помощи общего опросника PedsQL™ (J. Varni, 1999). Применялись варианты анкеты для детей 5–7 и 8–12 лет. Данный опросник содержит 23 вопроса, которые объединены в следующие шкалы: «Физическое функционирование» – ФФ (8 вопросов); «Эмоциональное функционирование» – ЭФ (5 вопросов); «Социальное функционирование» – СФ (5 вопросов); «Жизнь в школе» – ЖШ (3 или 5 вопросов в зависимости от возраста детей). Ответы на вопросы представлены в виде шкал Ликерта – это горизонтально расположенные варианты ответов на вопрос, каждому из которых соответствует цифра. После проведения шкалирования результаты оценки выражают в баллах – от 0 до 100 по каждой из 4 шкал опросника. Чем выше балл по шкале опросника PedsQL™ 4.0, тем лучше показатель качества жизни у детей. Кроме того, в процессе шкалирования получены суммарные баллы по психосоциальной компоненте качества жизни или психисоциальному функционированию (ПСФ) и суммарного балла по всем шкалам опросника – «Суммарная шкала» (СШ).
При статистической обработке применялся расчет критерия Фишера для малых групп и критерия Манна–Уитни. Статистическая обработка проведена с помощью программы «Биостатистика. Версия 4.03», значения менее 0,05 расценивались как значимые.

Результаты и их обсуждение
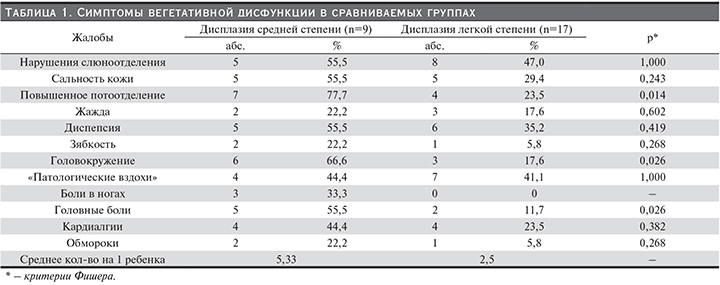
При сравнении характера и выраженности вегетативных проявлений в изучаемых группах установлено, что клинические симптомы вегетативной дисфункции значительно чаще выявляются в группе пациентов с более выраженными проявлениями мезенхимой дисплазии. Наиболее характерными клиническими проявлениями вегетативной дисфункции в группе больных ДСТ средней степени были повышенное потоотделение (77,7%), головокружение (66,67%), абдоминальные боли (55,5%), головные боли (55,5%), «патологические вздохи» (44,4%), кардиалгии (44,4%), обмороки (22,2%). В группе больных дисплазией легкой степени многие симптомы отмечались значительно реже. Наиболее часто выявлялись «патологические вздохи» (41,5%), нарушения слюноотделения (47%), кардиалгии (23,5%), повышенное потоотделение (23,5%), головные боли (11,7%), обмороки (5,8%). Среднее число симптомов на одного ребенка в 1-й группе составило 5,5, во 2-й было значительно меньше и составило 2,5. Результаты представлены в табл. 1.
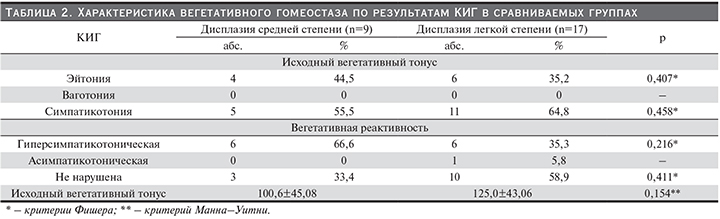
При оценке результатов КИГ установлено преобладание однонаправленных изменений вегетативного тонуса вне зависимости от степени дисплазии. Ведущими изменениями исходного вегетативного тонуса (ИВТ) были изменения по типу симпатико- и гиперсимпатикотонии. Данные изменения отмечены у 55,5% детей группы со средней выраженностиью дисплазии и у 64,8% – с низкой. В остальных случаях нарушений ИВТ выявлено не было. Изменения по типу ваготонии не выявлены ни в одном из случаев.
Изменения вегетативной реактивности, как известно, отражают состояние процессов адаптации. Преобладающими в двух группах были изменения по типу гиперсимпатикотонической реактивности, которые несколько чаще отмечались у пациентов с дисплазией средней степени выраженности, чем легкой, но статистически различия недостоверны – 66,6% и 35,3% соответственно. При этом асимпатикотонический тип вегетативной реактивности, соответствующий срыву процессов адаптации, отмечен только в 1 случае (5,8%) и у пациента с низкой степенью дисплазии. Результаты представлены в табл. 2.
Качество жизни на современном этапе является одним из интегральных методов оценки здоровья. Нами при оценке показателей качества жизни у детей с НДМП установлено значительное снижение показателей по всем шкалам вне зависимости от степени тяжести дисплазии. Наиболее низкие значения по шкале в сравниваемых группах получены по шкалам «Эмоциональное функционирование» (ЭФ) и «Жизнь в школе» (ЖШ). Также низкие баллы получены по шкале «Социальное функционирование» (СФ): в 1-й группе показатель составил 62,3±11,4 балла, во 2-й – 65,0±14,1 балла (р>0,05). Однако в обеих группах также низкими оказались показатели шкалы «Физическое функционирование», что в целом привело к низким значениям интегрального показателя качества жизни, значения которого составили 60,1±10,8 балла для больных дисплазией средней степени и 60,2±10,5 – для больных дисплазией легкой степени. Результаты представлены в табл. 3.
Заключение
Таким образом, клинические признаки вегетативной дисфункции чаще выявляются в группе больных ДСТ средней степени. Среднее число вегетативных симптомов на одного ребенка в данной группе составляет 5,5, против 2,2 в группе с дисплазией легкой степени тяжести. Результаты КИГ не зависят от степени выраженности ДСТ и характеризуются изменениями ИВТ по типу симпатикотонии, отмечающейся у 55,5% детей с ДСТ средней и у 64,8% детей с ДСТ легкой степеней. Преобладающими в двух группах были изменения по типу гиперсимпатикотонической реактивности, которые несколько чаще отмечались у пациентов с дисплазией средней степени выраженности, чем у пациентов с ДСТ легкой степени (66,6 и 35,3% соответственно). При изучаемых нозологиях на фоне ДСТ отмечается значительное снижение показателей качества жизни, при этом зависимости показателей качества жизни от степени ДСТ не выявлено.